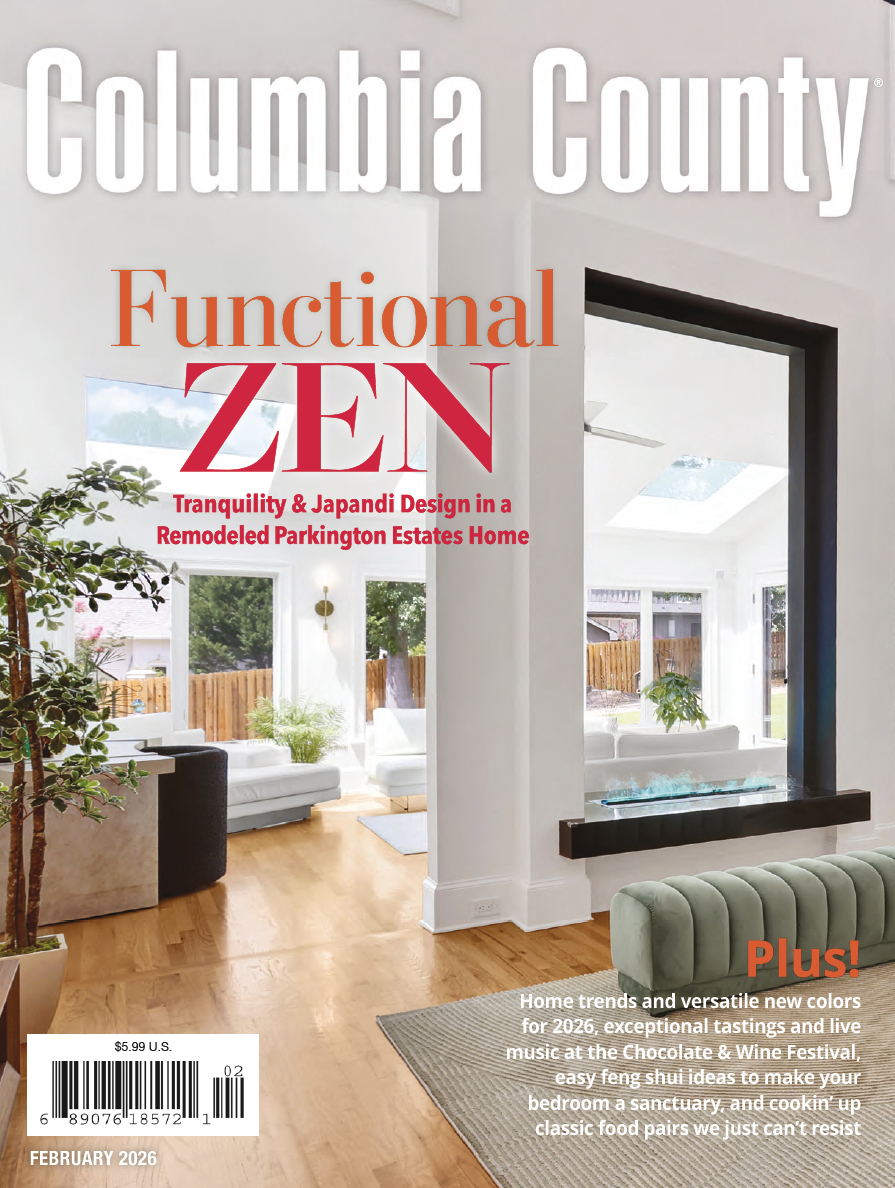
A Q&A with the chief medical officer of Augusta University Health System.
A Q&A with the chief medical officer of Augusta University Health System.
By now, all of us have heard more than we ever wanted to hear about COVID-19, the disease caused by the coronavirus. In early April, however, Dr. Phillip Coule, vice president and chief medical officer of Augusta University Health System, shared valuable information about the disease. At that time, the Martinez resident, who graduated from the Medical College of Georgia in 1996, said the area could pass its peak load of cases by late April. The Q&A has been edited slightly for clarity and space considerations.
Q: What is it like working in the hospital on the frontlines of the coronavirus pandemic?
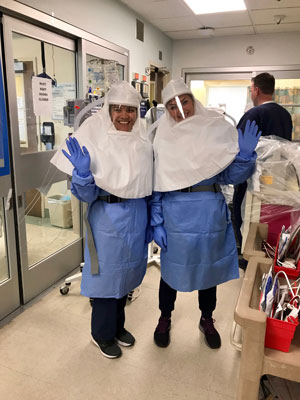
A: The team and our ICU staff are working incredibly hard, and they’re doing a fantastic job. There are lots of cases in the community as well as patients transferred from Albany. The patients in the ICU are very sick. We have two designated COVID-19 ICUs, but morale is high in the COVID-19 medical ward.
 Q: How was AU Health able to develop a test so quickly?
Q: How was AU Health able to develop a test so quickly?
A: If there’s a hospital version of “Doomsday Preppers,” we’re it. We have a leadership team that’s forward thinking. We have people who are constantly monitoring the latest trends in healthcare and what’s emerging. We were closely following the coronavirus developments in China and knew we needed to be ready. Everybody realized what could happen here and started preparing for the worst and hoping for the best. We started pursuing multiple testing platforms early on.
We knew the world was coming to town for Masters Week. Our goal was to have testing available by late March. We were pursuing different test platforms with different supply chains. We realize that Augusta is an international city and travel-associated cases were occurring early on in this. We realized Augusta needed to be prepared for a pandemic.
We didn’t make any changes after the Masters was postponed. This was widespread, and it accelerated our response.
Q: Which departments at the hospital have been affected by staff reductions?
A: These are unusual times. The shelter-in-place order is causing some people to defer some of their healthcare needs. That has decreased the need for surgeries that can be postponed, but we’re looking at ways to get patients back in the system.
Q: Can you tell if social distancing and sheltering in place are working?
A: We certainly do not want to let up now, but there is some reason for optimism, cautiously so. The combination of business closures, identifying and testing cases, and other measures have helped. There’s some evidence that we’re bending the curve. We need to keep doing what we’re doing.
Q: When do you think things might return to normal, and what will that look like?
A: My hope is that by the end of May or the beginning of June, we start to see things return to normal. We might see a loosening of mandatory closures. Restaurants might reopen with caution. We have to wait and see what happens before we get back to completely normal, but we don’t want to loosen up and then have things get out of control again.
We’ll feel a little better about the relaxation of the measures going into the summer. If we can get the ability to do antibody testing, it would allow us a better opportunity to know what’s really happening with this disease. Since some people only have mild symptoms, we haven’t been able to identify the true denominator. We hope to see signs of herd immunity where a lot of people don’t get the disease in the short term, making it harder for it to be transmitted.
Q: When do you think you will be able to start testing for antibodies?
A: Hopefully, by summertime. We are pursuing different options to test for antibodies, but we don’t have funding yet.
Q: How does this pandemic compare to anything else you’ve seen during your career?
A: This is unprecedented. I was involved in the response to 9/11, and I thought that was the only time I would see a disaster of that magnitude. Then I responded to Hurricane Katrina, and I thought that was the only time I would see another disaster of that magnitude. Then COVID-19 happened, and I’ve never seen anything like it.
It’s also remarkable to me how quickly people have adjusted to social distancing. We went from handshakes to fist bumps to elbow bumps to waving from six feet away. I’m hoping we go back to hugs. I’m hoping we go back to normal.
Q: What do you think things will look like in May?
A: I think we’ll know by then how we’ve weathered the storm.
Q: Is there a silver lining in any of this?
A: I’ve never seen a team pull together like the AU team has pulled together. We’ve done a world-class job in responding to this pandemic. That includes our pastoral staff, volunteer services and patient family services.
There are so many bright spots in this, I can’t count them all. Companies large and small have offered to donate masks. We can’t accept hand-sewn masks because there is so much variability in them, but we have accepted hand-made caps. My wife helped organize a sewing brigade to make the caps. They have been wildly popular. Everyone has loved them. People have fired up 3-D printers to print face shields.
We’ve had an incredible outpouring from the community. The support from the community has been great and very much appreciated. The parking lot prayers* were especially inspirational, and the food donations have helped to lift the morale of the staff.
Q: If there is one thing you would want people in the community to know, what would that be?
A: The importance of social distancing. It’s incredibly important for us to remember. Houses of worship and funerals will present the greatest risk to our most vulnerable populations. It may be necessary to modify things like that in the short-term so we can get back to normal in the long-term. And I’ve never been prouder of our entire team and the com